ABSTRACTS
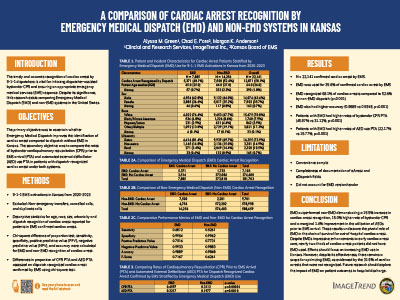
A Comparison of Cardiac Arrest Recognition by Emergency Medical Dispatch (EMD) and Non-EMD Systems in KansasAuthor: Alyssa Green, Chad E. Pore, Joseph A. House, and Morgan K. Anderson | | Associate Authors:
Introduction: The timely and accurate recognition of cardiac arrest by 9-1-1 dispatchers is vital for initiating dispatcher-assisted bystander cardiopulmonary resuscitation (CPR) and ensuring an appropriate emergency medical services (EMS) response. Despite its significance, little research exists comparing emergency medical dispatch (EMD) and non-EMD systems in the United States. Objective: To ascertain whether EMD improves identification of cardiac arrest compared to non-EMD in Kansas. Secondary Objective: To compare rates of bystander CPR prior to EMS arrival (PTA) and automated external defibrillator (AED) use PTA in patients with dispatch-recognized cardiac arrest under both systems. Methods: 9-1-1 EMS activations in Kansas from 2020–2023 were analyzed. Nonemergency transfers, canceled calls, and duplicate calls were excluded. Descriptive statistics were generated for age, race, sex, urbanicity, and dispatch recognition of cardiac arrest reported for patients in EMS-confirmed cardiac arrest. Chi-square difference of proportion test and accuracy were performed for EMD and non-EMD recognition of cardiac arrest. Differences in proportion of CPR PTA and AED PTA were assessed on dispatch-recognized cardiac arrest confirmed by EMS using a chi-square test. Results: Out of 970,362 activations, 22,141 were confirmed as cardiac arrest by EMS. Of these cardiac arrest patients, EMD was used for 35.6%. EMD recognized 68.1% of cardiac arrests compared to 52.6% by non-EMD dispatch (p < .001). EMD also had higher accuracy (0.9889 vs. 0.9848, p < .001). Additionally, patients with EMD had higher rates of bystander CPR PTA (45.97% vs. 31.12%, p < .001) and AED use PTA (22.17% vs. 19.77%, p = .001). Conclusion: EMD outperformed non-EMD, demonstrating a 15.5% increase in cardiac arrest recognition, 15.0% higher rate of bystander CPR, and a marginal 1.4% improvement in the utilization of AED PTA. These results underscore the pivotal role of EMD in the chain of survival for out-of-hospital cardiac arrest. Despite EMD’s impressive enhancements to early cardiac arrest care, nearly two-thirds of cardiac arrest patients did not use EMD. Efforts should focus on increasing EMD use in Kansas. However, despite its effectiveness, there remains a scope for optimizing EMD, as evidenced by the 31.9% of cardiac arrests that were not recognized. Future research should explore the impact of EMD on patient outcomes to hospital discharge.
|