ABSTRACTS
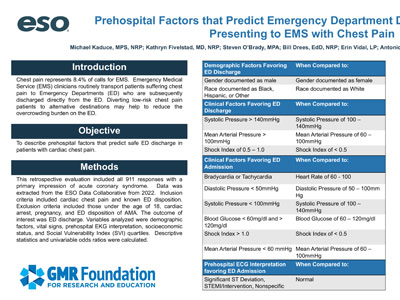
Prehospital Factors That Predict Emergency Department Discharge in Patients Presenting to EMS with Chest PainAuthor: Michael Kaduce, MPS, NRP | | Associate Authors: Kathryn Fivelstad, MD, NRP, Steven O’Brady, MPA, Bill Drees, EdD, NRP, Erin Vidal, LP, Antonio Fernandez, PhD, NRP, David Wampler, PhD, LP
Introduction Chest pain represents 8.4% of calls for EMS. EMS clinicians routinely transport patients suffering chest pain to emergency departments (EDs) who are then subsequently discharged directly from the ED. Diverting low-risk chest pain patients to alternative destinations may help to reduce the overcrowding burden on the ED. Objective To describe prehospital factors that predict ED discharge in patients with cardiac chest pain. Methods This retrospective evaluation included all 9-1-1 responses with a primary impression of acute coronary syndrome. The data source was the ESO Data Collaborative from 2022. Inclusion criteria included cardiac chest pain and known ED disposition. Exclusion criteria included pediatrics, cardiac arrest, pregnancy, and ED disposition of AMA. The outcome of interest was ED discharge. Variables analyzed were demographics, vital signs, prehospital EKG interpretation, socioeconomic status, and Social Vulnerability Index (SVI) quartiles. Descriptive statistics and univariable odds ratios were calculated. Results A total of 103,358 patients were included; 46% were admitted, 54% discharged. Females had a lower odds of discharge (OR: 0.80, 95% CI: 0.78–0.82). Blacks (OR: 1.38, 95% CI: 1.34–1.42), Hispanics (OR: 1.48, 95% CI: 1.41–1.55), and “other” races (OR: 1.45, 95% CI: 1.23–1.72) had increased odds of discharge than Whites. There was no difference between SVI quartiles. Clinical findings favoring discharge included systolic pressure (SBP) > 140 mm Hg (OR: 1.13, 95% CI: 1.10–1.16), mean arterial pressure (MAP) > 100 mm Hg (OR: 1.40, 95% CI: 1.36–1.43), shock index (SI) of 0.5–1.0 (OR: 1.23, 95% CI: 1.19–1.26). Clinical findings showing decreased odds of discharge included bradycardia or tachycardia (< 60 or > 100) (OR: 0.44, 95% CI: 0.42–0.46), (OR: 0.74, 95% CI: 0.72–0.76), respectively; diastolic hypotension (< 50 mm Hg) (OR: 0.36, 95% CI: 0.33–0.39), systolic hypotension (< 100 mm Hg) (OR: 0.42, 95% CI: 0.39–0.44), hypoglycemia (< 60 mg/dL) (OR: 0.41, 95% CI:0.35–0.48), or hyperglycemia (> 120 mg/dL) (OR: 0.60, 95% CI: 0.58–0.62), SI > 1.0 (OR: 0.63, 95% CI: 0.60–0.65), and MAP hypotension (< 60 mm Hg) (OR: 0.38, 95% CI: 0.35–0.43). Prehospital ECG interpretation was available on 64,689 patients. All abnormal interpretations had lower odds of discharge: ST changes (OR: 0.17, 95% CI: 0.11–0.25), STEMI/intervention (OR: 0.32, 95% CI: 0.30–0.34), and nonspecific (OR: 0.42, 95% CI 0.41–0.44). Conclusion More than half of patients transported by EMS for chest pain were subsequently discharged from the ED. Patient presentation, vital signs, and ECG interpretation provide support for down-triage to alternate destinations. Limitations include use of retrospective records and potential for residual confounding factors.
|