ABSTRACTS
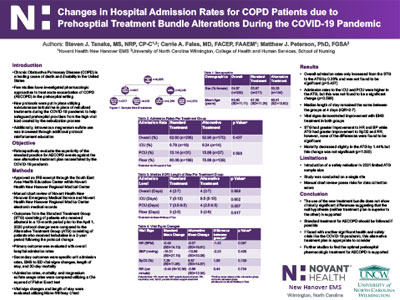
Changes in Hospital Admission Rates for COPD Patients Due to Prehospital Treatment Bundle Alterations During the COVID-19 PandemicAuthor: Steven Tanaka, MS, NRP | | Associate Authors: Carrie Fales, MD, Matthew Peterson, PhD
Introduction Chronic obstructive pulmonary disease (COPD) is one of the leading causes of death and disability in the United States; however, few studies have investigated the pharmacologic approaches in treating acute exacerbation events. Due to the COVID-19 pandemic, a prehospital service enacted new protocols to help keep providers safe from the high viral load created by nebulizing treatments. These protocols included using subcutaneous terbutaline in place of nebulized treatments and a push to utilize intravenous magnesium sulfate. Objective To retrospectively evaluate the superiority of the standard practice for treatment of COPD exacerbation against an alternative treatment plan put into place due to the COVID-19 pandemic. Methods Through retrospective chart review, the standard treatment group (STG) consisting of a 13-month period was compared to the alternative treatment group (ATG) consisting of a 2-year period following the protocol change on April 1, 2020. The primary outcome was evaluated through hospital admission rates. Secondary outcomes include specific department admission rates, vital signs changes, length of stay, and 30-day mortality. Magnesium sulfate use was also collected. Admission, mortality, and magnesium sulfate usage rates were compared using a chi-square or Fisher exact test. Vital signs changes and length of stay were evaluated using a Mann-Whitney U test. Results Overall admission rates only increased from the STG to the ATG by 0.36%, which was not found to be significant (p = 0.437). Admission rates to the higher level of care units were higher in the ATG; however, these were also not statistically significant. Overall, the length of stay remained the same between the groups with a median of 4 days (IQR 2–7) and was not found to have a significant change (p = 0.899). Mortality held steady with a slight reduction in the ATG by 1.44% but was not found to be significant (p = 1.000). Conclusion The use of this new treatment bundle did not show a clinically significant difference in overall admission rates, suggesting that the standard of care is reasonable. These findings also support the need for additional studies to find the optimal pharmacologic treatment of acute COPD exacerbation events in the prehospital setting.
|