ABSTRACTS
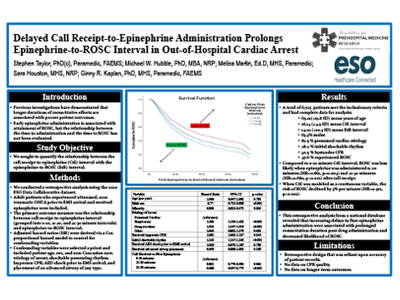
Delayed Call Receipt-to-Epinephrine Administration Prolongs Epinephrine-to-ROSC Interval in Out-of-Hospital Cardiac ArrestAuthor: Michael W. Hubble, PhD, MBA, NRP | | Associate Authors: Stephen Taylor, MHS, Sara E. Houston, MHS, NRP, Melisa Martin, EdD, MHS, Ginny K. Renkiewicz, PhD
Introduction Previous investigations have demonstrated that longer durations of resuscitative efforts are associated with poorer long-term patient outcomes. Aside from certain patient characteristics and interventions such as shockable rhythms and bystander CPR, little is known about factors influencing resuscitation duration. We hypothesized that delayed call-to-epinephrine administration (CtE) would increase the epinephrine-to-ROSC (EtR) interval and prolong low-flow duration. Objective To quantify the relationship between the call receipt-to-epinephrine and epinephrine-to-ROSC intervals. Methods We conducted a retrospective analysis using the 2020 ESO Data Collaborative dataset containing calls from January 2020 through December 2020. Adults with nontraumatic, witnessed arrests were included. End-of-event was defined as ROSC, termination of resuscitation, or hospital arrival without ROSC. A Cox proportional hazard model was used to determine the influence of CtE on EtR after controlling for potential confounders. Results Of the 6,725 patients analyzed, 1,897 (28.2%) presented with a shockable rhythm, 2,051 (30.5%) received bystander CPR, and 3,201(47.6%) attained ROSC. The mean CtE and EtR were 16.1 (±4.9) minutes and 14.02 (±10.3) minutes, respectively. After controlling for patient age, sex, minority status, arrest etiology, shockable rhythm, bystander CPR, advanced airway, and AED use, CtE was associated with decreased likelihood of ROSC (HR = 0.97 per minute, p < 0.001) when measured as a continuous variable. When stratified by 10-minute increments with 0–10 minutes as reference, CtE was negatively associated with ROSC (HR = 0.86, p < 0.001) and (HR = 0.68, p < 0.001) for the 11–20 and 21–30 minute categories, respectively (figure). Conclusion This retrospective analysis from a national database revealed that increasing delays in first epinephrine administration were associated with prolonged resuscitation duration and decreased likelihood of ROSC.
|