ABSTRACTS
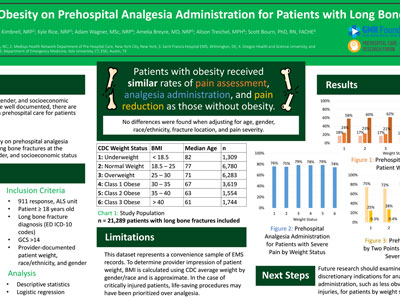
Impact of Obesity on Prehospital Analgesia Administration for Patients with Long Bone FracturesAuthor: Christopher Villani, EMT-B | | Associate Authors: Josh Kimbrell, NRP, Kyle Rice, NRP, Adam Wagner, MSc, Amelia Breyre, MD, NRP, Scott Bourne, PhD, RN, FACHE, Alison Treichel, MPH
Introduction Nearly half of American adults are obese. Numerous studies have demonstrated increased all-cause mortality, comorbidities, and clinician bias for patients with obesity in the hospital setting. While prehospital racial, ethnic, and socioeconomic disparities in pain management are well documented, there are few studies exploring disparities in prehospital care for patients with obesity. Objective To investigate the impact of obesity on prehospital analgesia administration for patients with long bone fractures at the intersection of race/ethnicity, gender, and socioeconomic status. Methods We conducted a retrospective analysis using the 2022 ESO Data Collaborative to analyze EMS records for 9-1-1 advanced life support transport of adult patients diagnosed with long bone fractures at the emergency department. Weight status was defined using the Center for Disease Control (CDC) body mass index (BMI) thresholds. BMI was inferred from provider-documented patient weight, race/ethnicity, and gender using CDC height averages. We compared rates of prehospital analgesic administration by weight status, accounting for race/ethnicity, gender, age, fracture location, scene/transport time, pain severity, and scene Social Vulnerability Index (SVI). Results Among the 21,289 patients identified with long bone fractures by 513 EMS agencies, 6,917 were classified as obese (32.5%). Patients with obesity received nearly equal rates of analgesia administration as those without obesity in cases where the patient reported a pain score of 6 or higher (77.4% [95% CI: 75.9–78.7%] vs. 76.9% [95% CI: 75.8–77.9%]). Furthermore, rates of documented pain screenings (84.4% [95% CI: 83.5–85.3%] vs. 83.0% [95% CI: 82.1–83.4%]), of severe pain (59.6% [95% CI: 58.3–60.8%] vs. 52.3% [95% CI: 51.4–53.2%]), and of pain reduction by two or more points from first to last pain score (70.9% [95% CI: 69.1–72.6%] vs. 73.1% [95% CI: 71.8–74.3%]) showed no significant changes by weight status. These results remained consistent after adjusting for race/ethnicity, gender, age, and scene SVI. Conclusion When reporting severe pain, patients with long bone fractures received analgesia at similar rates regardless of weight status. No disparities in analgesia administration by weight status were found after adjusting for race/ethnicity, gender, age, and scene SVI. Further research will examine the impact of more discretionary indications for analgesia administration for patients by weight status.
|